a positive test does NOT equal illness – but that’s the implication when we hear of a “spike in cases”
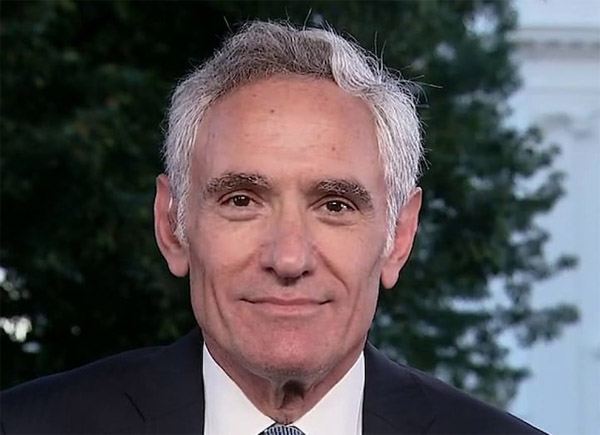
SLOPPY THINKING: Stanford’s Scott Atlas Rips Lockdown And Mask-Wearing Proponents For Denying Science And Ignoring Data
Dr. SCOTT ATLAS, Sr. Fellow Stanford University’s Hoover Institution
(Martha McCallum /Fox interview, June 8)
“The WHO yesterday said “it’s very rare” to have asymptomatic people transmit.”
“There’s this bizarre fixation on stopping cases, when cases are being defined by a positive test. The only thing that matters are the cases that are serious, that require hospitalization (or are fatal)…”
“When you look all over the world, countries that have opened, or partially opened, like Switzerland Netherlands Denmark Austria, they are NOT experiencing a higher number of hospitalizations or deaths. The same things goes for the (United) States… Florida, Texas, Georgia, they may have more cases but that doesn’t matter if it’s only people that are not going to have a significant problem with the infection. When we open up, we are going to have more infections if there is contagious disease present. When we test more, we’re going to have more cases. That is not the issue. The issue is to make sure we don’t have people who are going to get super sick or die, get infected. That’s the point. That is the denial of the science going on here with these closures.”
McCallum: asymptomatic spread… Why was that sold so strongly when obviously they didn’t know at the beginning whether or not it was true?
“I think what happens is we have a tremendous amount of fear… and the leadership of the States and all over the world sort of let that fear impact their decision making…. The science behind the six feet is completely sloppy, and what I would call lame.”
“Nobody gives, by the way, publicity to the WHO’s recommendation. ‘They do not recommend masks for the general public.’ Even in their updated note if you bother to read their whole technical note, they say that, and they are talking about the only time you wear a mask is if you are at risk, high-risk group in an area of widespread transmission of the disease and when you cannot be 3 feet away from someone. There is a tremendous amount of fear and there is a lot of smart people using what I would call sloppy thinking here.”
READ Article →
PCR test is prone to false positives, and does not prove someone has Covid-19 (or any infectious disease)
PCR Tests Show Positive Because They Respond to Genetic Material Present in All Humans →
“
New evidence shows that the controversial PCR test that tests for genetic material instead of the virus itself, is testing for a genetic sequence that is naturally found in humans. The sequence “CTCCCTTTGTTGTGTTGT” is an 18-character primer sequence found in the WHO coronavirus PCR testing protocol document. The primer sequences are the items that are amplified by the PCR process in order to designate a “positive” test result. The exact same 18-character sequence, in the same order, is also found on Homo sapiens chromosome 8! Chromosome 8 governs our intelligence and our immune system, especially resistance to cancer. This, alone, explains why there are so many false positive results.
Dr. Kaufman says no one has ever purified the virus, therefore, it cannot be proven that it is a new, never-been-seen before virus that is causing illness…
Dr. Kaufman says no one has ever purified the virus, therefore, it cannot be proven that it is a new, never-been-seen before virus that is causing illness…
Need To Know news
Are you infectious if you have a positive PCR test result for COVID-19? →
“
PCR detection of viruses is helpful so long as its accuracy can be understood: it offers the capacity to detect RNA in minute quantities, but whether that RNA represents infectious virus may not be clear. During our Open Evidence Review of oral-fecal transmission of Covid-19, we noticed how few studies had attempted or reported culturing live SARS-CoV-2 virus from human samples. This surprised us, as viral culture is regarded as a gold standard or reference test against which any diagnostic index test for viruses must be measured and calibrated, to understand the predictive properties of that test…
These studies provided limited data of variable quality that PCR results per se are unlikely to predict viral culture from human samples. Insufficient attention may have been paid how PCR results relate to disease. The relation with infectiousness is unclear and more data are needed on this. If this is not understood, PCR results may lead to restrictions for large groups of people who do not present an infection risk.
These studies provided limited data of variable quality that PCR results per se are unlikely to predict viral culture from human samples. Insufficient attention may have been paid how PCR results relate to disease. The relation with infectiousness is unclear and more data are needed on this. If this is not understood, PCR results may lead to restrictions for large groups of people who do not present an infection risk.
Centre for Evidence Based Medicine (CEBM)
The Trouble With PCR Tests →
“
Already in mid-March (2020), SPR explained that the highly sensitive PCR tests are prone to producing clinically false positive results and their individual predictive value may easily drop below 50%…
The issues with PCR tests are numerous:
The issues with PCR tests are numerous:
- There can be large-scale test kit contamination, as both the US and the UK (and several African countries) discovered during the early phase of the pandemic.
- There can be testing site or lab contamination, which has led to countless false positive results, school closures, nursing home quarantines, canceled sports events, and more.
- The PCR test can react to other coronaviruses. According to lab examinations, this happens in about 1% to 3% of cases if only one target gene is tested, as is the case in many (but not all)
- labs and as the WHO itself has recommended to avoid ambiguous positive/negative test results.
- The PCR test can detect non-infectious virus fragments weeks after an active infection, or from an infection of a contact person, as the US CDC confirmed.
- The PCR test can detect viable virus in quantities too small to be infectious.
Swiss Policy Research
International experts suggest that up to 90% COVID cases could be false positives →
“
An investigative piece by the New York Times has raised questions about the validity of the PCR type COVID mass-testing used in countries all around the world to identify COVID cases and to subsequently make policy decisions… The Westphalian Times has found that according to prominent epidemiology experts in the US and the UK, up to 90% of the Canadian COVID-19 cases could be false positives and that Canadians and their doctors are not given the important cycle threshold statistic when they get a positive result on a COVID test.”
Westphalian Times
People without symptoms (ASYMPTOMATIC) do not spread COVID-19, sick people do
“
In all the history of respiratory-borne viruses of any type, asymptomatic transmission has never been the driver of outbreaks. The driver of outbreaks is always a symptomatic person…
 Dr. Fauci: asymptomatic spread “never” drives outbreaks, only a “rare” asymptomatic person spreads it at all →
Dr. Fauci: asymptomatic spread “never” drives outbreaks, only a “rare” asymptomatic person spreads it at all →Coronavirus Disease 2019 (Covid-19) Situation Report – 73 →
“
There are few reports of laboratory-confirmed cases who are truly asymptomatic, and to date, there has been no documented asymptomatic transmission…
World Health Organization (WHO)
Asymptomatic cases ‘unlikely to be infectious’ in Ten Million Residents Wuhan →
“
The citywide nucleic acid screening of SARS-CoV-2 infection in Wuhan recruited nearly 10 million people, and found no newly confirmed cases with COVID-19. The detection rate of asymptomatic positive cases was very low, and there was no evidence of transmission from asymptomatic positive persons to traced close contacts. There were no asymptomatic positive cases in 96.4% of the residential communities…”
World Doctors Alliance
Household Transmission of SARS-CoV-2A – Systematic Review and Meta-analysis →
“
A total of 54 relevant studies with 77,758 participants reporting household secondary transmission were identified… Household secondary attack rates were increased from symptomatic index cases (18.0%; 95% CI, 14.2%-22.1%) than from asymptomatic index cases (0.7%; 95% CI, 0%-4.9%)”
NOTE: secondary attack (spread) from symptomatic cases was 18%, while with asymptomatic cases it was 0.7% – virtually none at all.JAMA Network OPEN
Covid-19 illness /hospitalization rates are similar to influenza (1-2%)
Hospitalization Rate → “
Initial estimates based on Chinese data assumed a very high 20% hospitalization rate, which led to the strategy of ‘flattening the curve’ to avoid overburdening hospitals. However, population-based antibody studies (see above) have since shown that actual hospitalization rates are close to 1%, which is within the range of hospitalization rates for influenza (1 to 2%).
The US CDC found that Covid-19 hospitalization rates for people aged 65 and over are “within ranges of influenza hospitalization rates”, with rates slightly higher for people aged 18 to 64 and “much lower” (compared to influenza) for people under 18.
In local hotspots like New York City, the overall hospitalization rate based on antibody studies is about 2.5% (19.9% or 1.7 million people with antibodies and 43,000 hospitalizations by May 2).
The much lower than expected hospitalization rate may explain why most Covid-19 ‘field hospitals’ even in hard-hit countries like the US, the UK and China remained largely empty.”
The US CDC found that Covid-19 hospitalization rates for people aged 65 and over are “within ranges of influenza hospitalization rates”, with rates slightly higher for people aged 18 to 64 and “much lower” (compared to influenza) for people under 18.
In local hotspots like New York City, the overall hospitalization rate based on antibody studies is about 2.5% (19.9% or 1.7 million people with antibodies and 43,000 hospitalizations by May 2).
The much lower than expected hospitalization rate may explain why most Covid-19 ‘field hospitals’ even in hard-hit countries like the US, the UK and China remained largely empty.”
Swiss Policy Research
Covid-19 Overview (facts) →
Covid-19 Deaths Over-Reported →
